On an August morning in 2008, Tony Wyss-Coray sat in a conference room at the Veterans Affairs hospital in Palo Alto, California, waiting for his lab’s weekly meeting to begin. Wyss-Coray, a professor of neurology at Stanford University, was leading a young group of researchers who studied ageing and neurodegeneration. As a rule, the gatherings were forgettable affairs â€" the incremental nature of scientific progress does not lend itself to big surprises. But a lab member scheduled to speak that day had taken on a radical project, and he had new results to share.
Saul Villeda, an ebullient PhD student with slick black hair and a goatee, had spent the past year engrossed in research that called to mind the speculative medical science of the middle ages. He was investigating whether the old and frail could be rejuvenated by infusions of blood from the young. The hypothesis was not as absurd as it might sound.
Villeda had conducted pilot studies with pairs of surgically conjoined mice that shared a blood supply for several weeks. Young mice received blood from older mice, and old mice received blood from younger ones. Villeda wanted to see the effect on their brains. Neurons in ageing brains lose their connections and start to die off; ultimately, the brain shrinks and becomes less effective. A region called the hippocampus, crucial for memory and learning, is one of the first to deteriorate with age, causing people’s memories and thought processes to falter.
Villeda’s work took skill. A mouse brain is the size of a peanut. To remove one for inspection is not difficult, but Villeda then had to cut each brain into wafers 1/25th of a millimetre thick using a cryomicrotome, a machine that resembles a benchtop deli slicer. Villeda took multiple slivers from about 40 mice and then stained them with a dye that binds to newborn neurons. Under a microscope the baby brain cells stand out like little brown trees.
The day before the lab meeting, Villeda and his colleague Kurt Lucin arrived early for work. With a small paintbrush, Villeda swept each brain slice, one after another, onto a microscope slide, and counted the tiny brown tree shapes. It took hours: he had about 200 slivers to inspect, from old and young mice. After totting up the newborn neurons in each section, he tapped the number into a statistics program. He finished after 10pm.
Though it was late, Villeda made Lucin stay with him to crunch the numbers. “It had been such a long experiment. I thought, if it doesn’t work, he’s here. We can go and grab a drink,†Villeda told me recently. He clicked a button on the screen marked “analyseâ€. The statistics program took all the data and calculated the average number of newborn neurons in the brains of each group of mice. A moment later, bar charts popped up on the screen.
Villeda got three hours’ sleep that night. The next morning, he stood up at the lab meeting and revealed to his colleagues what young blood did to the ageing brain. “There was a palpable electricity in the room,†Wyss-Coray recalled. “I remember seeing the images for the first time and saying, ‘Wow.’†Old mice that received young blood experienced a burst of brain cell growth in the hippocampus. They had three to four times as many newborn neurons as their counterparts. But that was not all: old blood had the opposite effect on the brains of young mice, stalling the birth of new neurons and leaving them looking old before their time.
The other scientists in the room were stunned. Some were sceptical. Could it be real? “This could be big,†said Wyss-Coray. “If an old mouse starts to make more neurons when you give it young blood? That is amazing.â€
Since that meeting seven years ago, research on this topic has moved on dramatically. It has led some to speculate that in young blood might lie an antidote to the ravages of old age. But the apparent rejuvenating properties of young blood must be treated with healthy scepticism. The hopes they raise rest solely on mouse studies. No beneficial effects have ever been proven in humans. Then again, no one has ever looked.
That is about to change. In October 2014, Wyss-Coray launched the first human trial of young blood. At Stanford School of Medicine, infusions of blood plasma from young people are being given to older people with Alzheimer’s disease. The results are expected at the end of the year. It is the greatest test yet for the medical potential of young blood.
* * *
For much of history, people sought to halt ageing to achieve immortality â€" or at least to live for hundreds of years. These days, scientists tend to have more modest aims. In wealthy nations, basic healthcare and medical advances have driven up lifespan for the past century. Five years from now, for the first time in human history, there will be more over-60s than children under five years old. In 2050, two billion people will be 60 or older, nearly double the number today.
Behind that statistic lies a serious problem. People are living longer, but they are not necessarily living better. The old struggle with chronic conditions, often many at once: cancer, respiratory disease, heart disease, diabetes, arthritis, osteoporosis, dementia.

Medical researchers tend to tackle these diseases separately. After all, the illnesses are distinct: cancer arises from mutated DNA; heart disease from clogged up blood vessels; dementia from damaged brain cells. The biological processes that underpin the pathologies vary enormously. Each, then, needs its own treatment. Yet some researchers take another view: the greatest driver of disease in old age is old age itself. So why not invent treatments for ageing?
The idea has caught on, though it is still far from mainstream. Google’s secretive Calico operation, founded in 2013, is putting hundreds of millions of dollars into anti-ageing research. Craig Venter, the genetics entrepreneur, has launched a company called Human Longevity to find the genes that lead to long life. Meanwhile, scientists have asked the US Food and Drug Administration to approve trials of well-known drugs, such as the diabetes treatment, metformin, in the hope of uncovering anti-ageing effects.
Scientists may never halt the process entirely: ageing is an opaque and complex mingle of molecular pathways. But they might learn how to stop changes that underpin the worst chronic diseases. They want to extend healthspan, not lifespan. The stakes are enormous. Over the next decade, the cost of dementia care in Britain alone will rise to £24bn, a 60% increase on the cost in 2007. Last year, the World Health Organisation called the rise in chronic illness due to the greying population a major public health challenge.
Wyss-Coray is not the first person to wonder whether the answer to the problem of ageing might lie in human blood. One of the first physicians to propose blood transfusions to rejuvenate older people was Andreas Libavius, a German doctor and alchemist. In 1615 he proposed connecting the arteries of an old man to those of a young man. He had high hopes for the procedure. “The hot and spirituous blood of the young man will pour into the old one as if it were from a fountain of youth, and all of his weakness will be dispelled,†he claimed, in an account told in the Textbook of Bloodbanking and Transfusion Medicine by Sally Rudmann. It is unclear how it turned out; there is no record of the transfusion happening.
The fledgling years of the Royal Society, founded in London in 1660, witnessed some of the earliest experiments in blood transfusion. When Robert Boyle, one of the society’s founders, compiled a wishlist of scientific projects, the top entry was “The prolongation of lifeâ€. That might be achieved, he hoped, by replacing old blood with new.
Progress in science takes more than hope. With no knowledge of blood groups or coagulation factors, the early transfusion experiments were deadly. Before long, the procedure was banned, first in France, and then England. The pope endorsed the bans in 1679, and transfusion all but ceased for a century. When advances in medicine allowed its return, the emphasis was on healing the sick, not helping the aged.
It is 400 years since Libavius proposed that young blood could rejuvenate older people. At the time, the idea was radical and dangerous. Even though modern science has made blood transfusions safe, blood remains a mysterious fluid: it ferries more than 700 proteins and other substances around our bodies; many are known, but what they do is less clear. Wyss-Coray suspects that among them are factors that orchestrate the ageing process. If scientists can understand how they work, the ageing process might be laid bare. It could be slowed down, or perhaps even reversed.
* * *
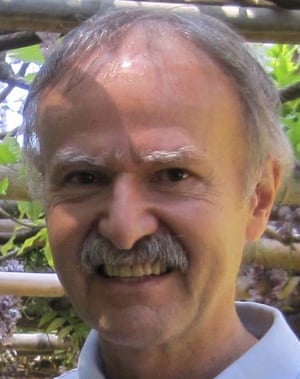
When Wyss-Coray was in his 20s and 30s, he did not much care about ageing. “You have no understanding of what the problems are,†he recently told me, in his soft Swiss-German accent. Sitting in his office at the Veterans Affairs hospital, surrounded by books on immunology and biology, Wyss-Coray was fashionably unshaven, with a crop of blonde hair and lively blue eyes framed by dark rimmed glasses. “Now I see that the brain starts to slow down. I’m not as quick any more at grasping things, or remembering faces. I used to see a person for a few minutes and I’d remember their face. I couldn’t understand how they’d not remember who I was. And now it happens to me. It annoys the crap out of me.â€
For Wyss-Coray, ageing has become much more than a personal bugbear. In 2014, the prestigious US journal, Science, named his work on young blood one of its breakthroughs of the year. He is regularly invited to give talks at conferences and the world’s top universities; in January, he spoke at the World Economic Forum in Davos. “In almost every talk I give, people make comments or jokes about vampires.†He slumped back in his chair and groaned. Another question also crops up: “I have people asking me, ‘Are you taking young blood?’†He assured me that he was not, and screwed up his face in horror, but it’s easy to see why they ask; he looks much younger than his 50 years.

Wyss-Coray was the first in his family to go to university. From the start, he set his sights on a career in the US. In 1993, he began as a postdoctoral fellow at the well-regarded Scripps Research Institute in La Jolla, California, studying HIV-related dementia. The work led to Alzheimer’s research, focusing on how the immune system played a role in the disease. In 2002, he joined Stanford University’s medical school, where he remains a faculty member.
Much of Wyss-Coray’s research on Alzheimer’s used mice that were genetically modified to develop the disease. This kind of experimentation has major limitations. Alzheimer’s mice mimic the forms of disease that run in families because of specific mutations, but they cannot tell us much about the origins of the sporadic forms of Alzheimer’s, which account for 99% of human cases. “People always joke: if you’re a mouse and you have Alzheimer’s, we can cure you, no problem,†Wyss-Coray told me. For humans, however, nothing so far has worked.
Frustrated by the limitations of his experiments, Wyss-Coray looked for better ways to understand how the disease first arose in humans. Brain scans and cognitive tests were out â€" neither revealed anything about disease at the molecular level. Nor would it make sense to study the brains of the dead, as scientists had traditionally done: the subtle neurological changes that lead to Alzheimer’s are set in motion two or three decades before patients are diagnosed, which meant old brains told you how bad the rot got, but not how the rot got started.
Wyss-Coray wondered if blood might hold the answer. Human blood travels 96,000 kilometres along the arteries, veins and capillaries of the circulatory system. It circulates through every organ. What if blood picked up information as it streamed around the body? What if its molecular makeup reflected the state of the brain, as it aged and changed with disease?
He assembled an international team of two dozen scientists to test the idea. They analysed blood plasma from more than 200 Alzheimer’s patients, and compared the profiles with those from healthy people. The findings, published in 2007, made headlines around the world. By measuring the levels of certain proteins in plasma, Wyss-Coray’s team believed they had found an accurate way to diagnose Alzheimer’s years before it began to take its toll. Wyss-Coray set up Satoris, a private company, to commercialise the research.
The study was too good to be true. Wyss-Coray’s later efforts to develop the test showed it was unreliable. In the course of this work, however, he had come across something intriguing. He noticed that in healthy people, the levels of certain proteins in blood fell with age. By 20 years old, most had already dropped steeply. Meanwhile, the levels of other proteins ramped up. Some doubled or tripled in old age. What the changes meant, no one knew.
* * *
One floor up from Wyss-Coray’s lab is the office of Thomas Rando, a neurologist and deputy director of the Stanford Center on Longevity. On his desk sits a small display of chemistry lab glassware and dozens of miniature figurines of the New York Giants. It was Rando who hired Wyss-Coray in 2002. “Tony is incredibly creative,†Rando told me. “He thinks about neuroscience in the context of the whole organism, as opposed to someone who has tunnel vision of the brain.â€
In 2005, Rando oversaw a series of important experiments that would become closely intertwined with Wyss-Coray’s work. The question Rando wanted to investigate centred on stem cells. The body’s tissues need stem cells to remain healthy and in good working order, but in older people, stem cells stop doing their job â€" this is why wounds heal so much slower as we age. Rando wondered whether stem cells failed in old animals because they no longer got the right signals. What if something in young blood turned them back on again? Perhaps he could make older people heal as fast as young ones.
Rando’s experiments involved an unsettling but remarkable procedure in which mice were cut along the flanks and sewn together, wound-on-wound. This procedure, pioneered by the 19th-century French physiologist Paul Bert, is known as parabiosis. Bert’s work on conjoined rats demonstrated that, once their wounds had healed, the animals developed a single, shared circulatory system.
For a long time, experiments involving parabiosis were gruesome. In 1956, Clive McCay, an American gerontologist at Cornell University who was pursuing a similar line of research to Wyss-Coray, described his own attempts to conjoin rats in the Bulletin of the New York Academy of Medicine. “If the two rats are not adjusted to each other,†he wrote, “one will chew the head of the other until it is destroyed.†Grim though it was, McCay’s work hinted that young blood might have rejuvenating properties.
Though other scientists took up McCay’s experiments and got similarly encouraging results, the work was effectively abandoned in the 1970s. Not knowing what to make of their findings, researchers moved on to other projects. Only when parabiosis was resurrected at Stanford did scientists start to make sense of the anti-ageing effects.
Parabiosis is different today: ethics committees are strict and the surgical procedure has improved. The animals are genetically matched, so there is no risk of immune rejection. Once they have recovered from the operation, paired animals tend to eat normally and to make nests together. But the procedure is still disturbing â€" it would be a stretch to call the animals happy.
Scientists in Rando’s lab joined old and young mice for five weeks and looked at how well they repaired little tears in muscle tissue. The young blood activated stem cells in the old mice that swiftly regenerated their damaged muscles. The young mice, however, fared worse for their exposure to old blood. Their stem cells became sluggish, and their tissues healed more slowly. Rando saw hints of another effect too, but needed more evidence before he could publish: the old mice had begun to grow new brain cells.
The results led Wyss-Coray and Rando to collaborate. The kinds of proteins Wyss-Coray had seen rise and fall in blood were known to have effects on biological processes. What if they had driven the changes Rando had seen in muscle? Might they similarly revitalise the brain? Rather than being mere signatures of age, the proteins might be chemical cues for the ageing process itself.

Wyss-Coray asked his PhD student Saul Villeda to investigate. Villeda grew up in Pasadena on the outskirts of Los Angeles. His parents had immigrated illegally from Guatemala in the 1970s, and took jobs in factories, or as janitors. They became legal residents when Saul was a boy. Villeda had not planned on being a scientist when he went to college at the University of California in LA. But he enjoyed physiology classes: “I instantly fell in love with research,†he told me. “The idea that you were investigating something completely new and that you could come up with your own experiments to figure things out was amazing.†When he told his parents he wanted to be a university scientist, they didn’t really know what he meant. “I took them to my undergraduate lab to show them what a scientist looked like,†he said. “I think that really helped them understand.â€
After Villeda presented his work on conjoined mice to Wyss-Coray at the lab meeting in August 2008, he went on to look at proteins in old and young blood. He found that the old mice, like old humans, had high levels of a protein called CCL11 in their blood. If you injected CCL11 into young mice, their learning and memory declined. The protein hampered the growth of new neurons. The young mice struggled to remember the location of a hidden platform in a water maze, and took longer to recognise a place where they had received a small but unpleasant electric shock. Villeda published the landmark research in 2011.
But the study failed to answer a major question: could proteins in young blood restore the mental capacities that old animals lost? Testing this was by no means easy. A mouse’s wits can be examined in a water maze, but two mice sewn together? It would be impossible to know how much one had led the other. Wyss-Coray believed that rather than experimenting with conjoined mice, the only option was to take blood from young mice, strip out the blood cells, and inject the plasma into old ones. This, too, was difficult. One mouse yields about 200 microlitres of plasma, the yellowish fluid that contains all the proteins. That is enough for two injections into another mouse. For an experiment that requires 10 injections into 10 old mice, you need to siphon the blood from 50 young mice.
Villeda was reluctant to do the experiment. He didn’t think it would work. But he changed his mind when he performed electrical measurements on slices of brain tissue and found that exposure to young blood strengthened the connections between neurons that had weakened in old mice. He went ahead with the plasma injections. Each mouse had one injection every three days for 24 days. The plasma came from three-month-old mice, the equivalent of human beings in their 20s, and went into 18-month-old mice, the equivalent of a human in their 60s.
The results were dramatic. Old mice given young plasma jabs aced the water-maze test, and quickly remembered the cage where they had earlier received an electric shock. They performed like mice half their age. “That time, I showed Tony the data one-on-one,†Villeda told me. “I was freaking out. I said: ‘I have to see this again.’â€
Not everyone was impressed. The journal Nature rejected the study in 2012; its reviewers felt the work was not a big enough leap forward. So Wyss-Coray and Villeda sent it along to a sister publication, Nature Medicine. The editors there wanted to know precisely how young blood helped old mice. Villeda, who had just opened his own lab at the University of California in San Francisco, said he would find out.
Villeda looked at how young blood altered the way genes are expressed in old mice. He noticed a stark difference among genes that help neural connections strengthen and weaken, a process crucial for learning and memory. In normal ageing, the genes that control this “synaptic plasticity†become less active. Young plasma jabs ramped the gene activity back up again.
From the pattern of genes affected, Villeda traced the mechanism back to a master regulator in the brain, a protein known as CREB, which behaves like a switch that turns on many genes at once, and is instrumental in memory and learning from birth. To confirm young plasma was working through CREB, Villeda’s PhD student Kristopher Plambeck designed a virus that turned the master regulator off. When they injected the virus into old mice, young plasma had a much reduced effect on their brains. The animals performed better, but only slightly. It showed that young plasma worked through CREB, though not exclusively.
The study was published in Nature Medicine in 2014. Immediately, emails flooded in to Wyss-Coray’s inbox. Alzheimer’s patients wanted infusions of young blood. So did numerous aged billionaires. One, who flies around in a jet with his name emblazoned on the side, invited Wyss-Coray to an Oscars after-party this year. (He didn’t go.) Another correspondent wrote with a more disturbing offer: he said he could provide blood from children of whatever age the scientists required. Wyss-Coray was appalled. “That was creepy,†he said.
Wyss-Coray and Villeda were not the only scientists making headway in this area. Two members of the team behind Rando’s 2005 paper on stem cells had moved to the University of California, Berkeley, where they found that oxytocin, often called the love hormone, rejuvenated old muscle tissue. Another, Amy Wagers, had begun working at Harvard. She showed that when given young plasma, old mice regained their stamina. On a treadmill, the treated mice ran for an hour on average, compared with only 35 minutes for untreated ones.
Wagers picked out one factor, known as GDF11, as a rejuvenating protein in young blood. In Villeda’s most recent paper, published in July 2015, he found a second factor, B2M, which peaks in the blood of old mice, as it does in old humans: when injected into young mice, B2M impairs their memories.
The studies all point in one direction. Among the hundreds of substances found in blood are proteins that keep tissues youthful, and proteins that make them more aged. Wyss-Coray has a hypothesis: when we are born, our blood is awash with proteins that help our tissues grow and heal. In adulthood, the levels of these proteins plummet. The tissues that secrete them might produce less because they get old and wear out, or the levels might be suppressed by an active genetic programme. Either way, as these pro-youthful proteins vanish from the blood, tissues around the body start to deteriorate. The body responds by releasing pro-inflammatory proteins, which build up in the blood, causing chronic inflammation that damages cells and accelerates ageing.
“This opens an entirely new field. It tells us that the age of an organism, or an organ like the brain, is not written in stone. It is malleable. You can move it in one direction or the other,†says Wyss-Coray. “It’s almost mythological that something in young organisms can maintain youthfulness, and it’s probably true.â€
* * *
As a business proposition, the transfusion of young blood raises all kinds of fears. It raises the spectre of a macabre black market, where teenagers bleed for the highest bidder, and young children go missing from the streets. Then there is the danger of unscrupulous dealers selling fake plasma, or plasma unsafe for human infusion. The fears are not unfounded: health has become one of the most lucrative sectors for criminals and con artists.
Havocscope, an online database, tracks the latest prices of all manner of black market goods and services. For $600 you can buy an AK-47 in Europe. A rhino-horn dagger will cost you $14,000. The services of a group of former military snipers? That will be $800,000. The list includes human organs too, mostly lungs, kidneys and livers. Today, a healthy seller can expect about $5,000 for their kidney. The organ broker who handles the deal can make a hefty profit, selling it on for $150,000 to a wealthy patient who needs a transplant.
In some countries, there is already a legal market for blood plasma. In the wake of the BSE crisis of the 1990s, plasma donations are not used in the UK. But in the US, donors can make $200 a month (plus loyalty points) from plasma donations. The fresh plasma is separated from the blood, and the red blood cells returned to the bloodstream, in a sitting that lasts 90 minutes. The plasma is used in medical procedures, to treat coagulation disorders and immune deficiencies. The business is completely legitimate, but if young plasma is proved to have anti-ageing effects, the risk of backstreet operators setting up will soar. When I asked Wyss-Coray if the prospect worried him, he looked serious. “Absolutely,†he said. “There are always going to be nutcases.â€
These are worst-case scenarios. The Stanford trial may find that simply injecting young plasma into old people has little or no effect. Wyss-Coray confesses that he suspects as much. He believes that rejuvenating older people might take a more potent brew than natural plasma. He has in mind a concentrated blend of 10 or 20 pro-youthful factors from young blood, mixed with antibodies that neutralise the effects of ageing factors found in old blood.
In January 2014, Wyss-Coray set up Alkahest, a company that aims to separate plasma into its constituent parts, and combine them into a potent, rejuvenating cocktail. In Silicon Valley, scientists frequently launch start-up companies on the back of early-stage research â€" an alignment of the commercial and the scientific that some researchers still frown upon. Sergio Della Sala, a professor of human cognitive neuroscience at the University of Edinburgh, warns that creating a business before the science is done can raise a conflict of interest. “Science should first understand then sell,†he said. “We should always be skeptical when these two factors are reversed.â€
Wyss-Coray formed Alkahest with Karoly Nikolich, an entrepreneur and neuroscientist at Stanford, who immigrated to the US from Hungary in the 1970s. I met Nikolich at his office in Menlo Park in February. He has thin hair, a full grey moustache and a mind filled with stories. Sat at a table on the sun-drenched roof terrace, Nikolich, handed me an Alkahest business card. The company logo is a blue droplet. Inside it is a golden disc.
Nikolich got to know Wyss-Coray in 2005. He had taken on the job of executive director of the Neuroscience Institute at Stanford University and over the years, Nikolich kept tabs on Wyss-Coray’s progress â€" from the Alzheimer’s blood test to the rejuvenating properties of young blood. But it wasn’t until spring 2012 that plans to form a company emerged. Nikolich had flown to Hong Kong to visit the family of Chen Din-hwa, a Chinese billionaire known as the King of Cotton Yarn. Three years earlier, Chen had died, aged 89, with Alzheimer’s disease. His grandson told Nikolich that towards the end of his life, Chen barely recognised his own family. Then he had a plasma transfusion for an unrelated condition, which seemed to have a spectacular effect. His mind was clearer. He was suddenly cogent.
Nikolich told them about Wyss-Coray’s research and the potential for plasma-based therapies that revitalised the ageing brain. Before long, the conversation turned to starting a company. The family invested a year later. The money got Alkahest established and ready to launch the first human trial of young plasma.
Alkahest’s ultimate goal â€" to identify the key proteins in plasma that rejuvenate or age human tissues and then manufacture a product that uses them â€" could take 10 to 15 years. In the near term, the company has another strategy. Earlier this year, the Spanish blood products firm, Grifols, pledged $37.5m for a 45% stake in Alkahest. With another $12.5m, the company will bankroll more research in exchange for rights to Alkahest’s first products. Over the next two years, Alkahest will take human plasma and divide it into fractions that are rich in different proteins. Each fraction will then be tested in mice to see if they boost brain function. Any that do will be swiftly introduced into human trials and developed into the first generation of products.
And what then? One enormous obstacle for hopes of plasma therapy is the limited supply. In a rough extrapolation from the mouse studies, Nikolich estimates that the globe’s entire plasma supply would be sufficient for only half a million of the world’s 15 million Alzheimer’s patients. “That means big questions about who gets treatment and who does not,†he said.
* * *
A short drive from the Palo Alto Veterans Affairs hospital is Stanford University’s School of Medicine, where the Alkahest trial is running. The woman in charge of the trial is Sharon Sha, a specialist in behavioural neurology who spends much of her time with patients who have Alzheimer’s. When I visited in February, Sha, a cheery woman with dark shoulder-length hair, was running late for a meeting in her third-floor office. But she was delayed for good reason: she had been infusing young plasma into an Alzheimer’s patient enrolled on the trial â€" a procedure that cannot be rushed.
The Alkahest trial is small. Sha can enrol only 18 people aged 50 to 90 with mild to moderate Alzheimer’s disease. Each receives a unit of young human plasma or saline once a week for four weeks. They have the next six weeks off, then have four more weeks of infusions. Those who had plasma first time around get saline and vice versa. The process is blinded, so neither the patients, nor their carers, nor Sha herself, know who is receiving what. Throughout the trial, doctors will look for cognitive improvements. Only at the end of the trial, as soon as October this year, will Sha analyse the findings.

Big questions lie ahead. Even if none of the patients benefit from young plasma, the research is far from finished. The plasma for the trial comes from donors under 30, and it may not be potent enough. The patients on the trial have dementia already, and may be too far gone to rescue.
Earlier this year, John Hardy of University College London, who is the most cited Alzheimer’s researcher in Britain, saw Wyss-Coray’s latest data at a meeting in London. “It’s really interesting work,†he told me. “It’s woken everybody up.†Nonetheless, Hardy is cautious; he suspects that young plasma will be less effective in people than in mice, because people live so much longer, and in far more varied environments. But, he said: “I would guess this will still point us towards pathways involved in ageing more generally.â€
If patients improve with infusions of young plasma, scientists will be ecstatic. But the finding would need to be replicated, ideally at other hospitals, and in more patients, in order to convince researchers. If any benefits stand the test of time, the studies will move on, to tease out the best doses and ages at which to give plasma, how patients’ brains change, and whether improvements make a real difference to the life of someone who can no longer recognise their own family.
Then there is safety. Toying with the ageing process might backfire. Rando is concerned that pumping pro-youthful proteins into people for years could end up giving them cancer. Wyss-Coray agrees it is a worry, but points out that long-term growth hormone therapy appears to be safe. “We just don’t know yet whether or not it will be a problem,†he said.
Rando is more upbeat about infusing patients with pro-youthful proteins for short periods. An elderly person having surgery might get an infusion to help them heal like a teenager. “Let’s say it works. If you can target tissues and improve wound healing in older people, that would be a feasible approach. It would not be about making 90-year-olds younger, or having people live to 150. It’s about healthy living, not longer living,†he said.
In the 20 years that Wyss-Coray has lived in the US, his attitude to ageing has swung from disinterest to fascination. Why does a mouse live for three years and a human for 80? He sees its effects on a personal level too. He gets frustrated when a word fails to come as quickly as it once did, but knows how much worse it must be for people noticing the early signs of dementia: their words and memories slipping away into the gloom.
The carers of the patients enrolled in the young-blood trial keep journals to record how well the patients are doing. Among their pages may be signs of hope, that perhaps in the days after an infusion, a patient does a little bit better. “If it actually works? That would be huge. Every patient would want it,†Wyss-Coray said. He smiled. “I’d probably have to turn off my email and go somewhere else.â€
• Follow the Long Read on Twitter: @gdnlongread
No comments:
Post a Comment